Specimen Collection and Transport Procedure for CSF Neurotransmitters
CSF neurotransmitters is a send-out test to the Division of Chemical Pathology, Queen Mary Hospital (QMH).
Instructions for Clinicians
- The clinicians must contact QMH Duty Biochemist at (Tel: 2255 3174) for test arrangement. Once the test arrangement is confirmed, the clinicians should also call PWH Duty Biochemist at least one day before the procedure.
- Patient preparation:
- Before CSF collection, avoid drugs which affect neurotransmitter turnover, e.g. serotonin reuptake inhibitors (SSRI) / serotonin-dopamine reuptake inhibitor (SDRI), mono-amine oxidase inhibitors (MAOI), catechol-o-methyltransferase inhibitors, etc., only if this will not cause any clinical deterioration.
- Any patient who is on L-DOPA treatment should have the drug stopped for at least 3 to 4 days before analysis of neurotransmitters for diagnostic purpose only. No drug modification is necessary if the lumbar puncture is for biochemical monitoring after treatment. The need for drug modification is decided on an individual basis, taking into the account that clinical deterioration may occur with exacerbation of the movement disorder if L-DOPA has to be stopped for diagnostic purpose i.e. may need hospitalisation for close observation.
- Ideally, CSF should be collected at a time when symptoms are the most severe. Otherwise, CSF specimens should be collected between 0800 and 1000 Hr in the morning before any medication is taken.
- Record the collection time on the request form.
- List all current medications on the request form.
- Take thermo-flask with ice blocks (in 4 °C) and CSF collection tubes (see Appendix) from the Rapid Response Laboratory, 3/F, Main Clinical Block and Trauma Centre, PWH (telephone: 3505 2363) 30 min before the collection of CSF specimens
- Label each collection tube with patient’s name and HKID.
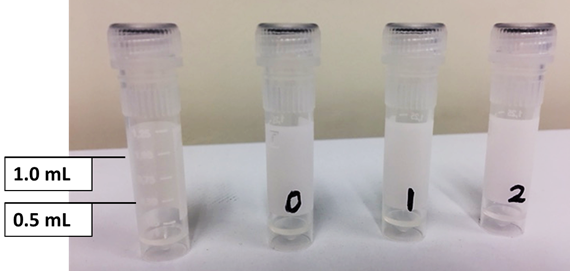
Collect the CSF sample into the respective plain microtubes provided by the laboratory, with the required volume, and label them from 0 to 2. Collect CSF into the tubes from the first drop in the order below. For other CSF investigation (if any), please collect after tube #2 and make the request(s) separately.
| Tube Number |
CSF Volume (mL) |
Investigation |
| 0 |
0.5 |
- |
| 1 |
0.5 |
CSF neurotransmitters (biogenic amines and 5-methyltetrahydrofolate) |
| 2 |
0.5 - 1.0 |
CSF neurotransmitters (pterins) |
- Due to the rostrocaudal gradient present in the spinal column, failure to follow the order of collection in the protocol below can lead to inaccurate results and misinterpretation. Therefore, never collect the CSF into one large tube and then aliquot into the micro-tubes.
- Place the CSF sample tubes and the handwritten specimen request form (please fill with a water-proof ball-pen) inside a double-compartment plastic bag separately and stick a gum label with patient’s name and HKID on the plastic bag.
- Put the plastic bag inside the thermo-flask and ensure that the sample tubes are surrounded by the ice blocks. Deliver the samples immediately to the Rapid Response Laboratory, 3/F, Main Clinical Block and Trauma Centre, PWH, in the thermo-flask with ice blocks provided by the laboratory.
- Blood-contaminated specimen will be rejected by QMH because haemoglobin may cause auto-oxidation of pterin. Please inform laboratory staff for special handling (i.e. centrifugation to remove the blood) if the CSF samples appear blood stained.
Appendix 1
 |
 |
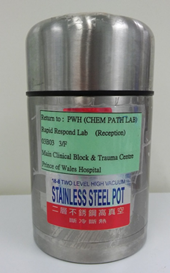
| Figure 1. Thermo-flask |
Figure 2. Specimens in plastic bag with 4 °C ice blocks placed inside the thermo-flask |
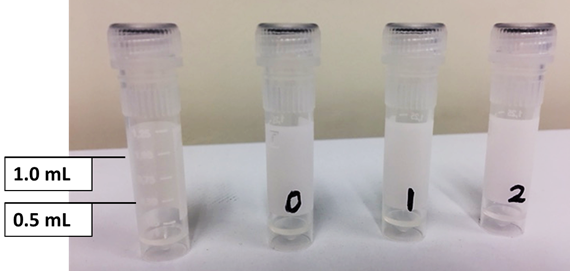 |
| Figure 3. CSF collection tubes (Fill up the specimen to the 0.5 mL and 1.0 mL marked line. Pre-label the three tubes as '0', '1' and '2' and collect the CSF samples in order.) |
Reference
Instructions for Collecting CSF for Neurotransmitters Analysis (MF 039, Last update: 20 March 2017) from the Division of Clinical Biochemistry, Queen Mary Hospital